Acute Ischemia of the Mammillary Bodies
- Background
- Mammillary bodies are a paired diencephalic structures located posterior to the hypothalamus and are part of the limbic system, key to the formation of episodic memory. It is formed by two nuclei; the lateral nucleus and the medial nucleus, the latter of which seems to have a greater role in memory.
- The mammillary bodies connect with other structures involved in the Papez circuit through the postcommissural fibers of the fornix, mamillothalamic tract, mammmillotegmental tract and mammillary peduncle. Lesions of the mammillary bodies can selectively disconnect them from the rest of the circuit, causing an alteration of the short-term memory.
- Mammillary bodies receive blood supply from perforators originating from proximal PCA (P1 segment) or posterior communicating artery.
- Clinical Presentation
- An isolated infarct of the mammillary bodies is rare but can result in acute amnesic syndromes.
- Once the episode resolves, persistent residual episodic memory failures may be seen.
- After stroke, the mamillary body may become atrophic. Mamillary body atrophy has rarely been reported in posterior cerebral artery (PCA) territory infarction.
- Key Diagnostic Features
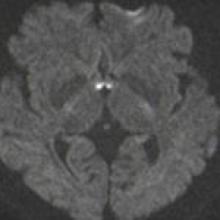
- As in any other ischemic lesion, there is restricted diffusion (high DWI signal with low ADC values) in the acute and early subacute phase, which later evolves with atrophy and increased water diffusivity.
- In the subacute phase, there may be contrast enhancement, so it may mimic a Wernicke's encephalopathy.
- Differential Diagnosis
- Infection/inflammatory process: In the acute phase, they can show T2 hyperintensity, but there is usually no diffusion restriction. They commonly involve the limbic system and the fornices.
- Transient epileptic amnesia: Electroencephalogram monitoring will show epileptiform activity.
- Postconcussive syndrome: Secondary to nonpenetrative trauma. Swelling or hemorrhage of the mammillary bodies may be seen at early stages.
- Multiple sclerosis: Demyelinating plaques in other locations are usually seen.
- Wernicke encephalopathy: Associated clinical features as ophthalmoplegia, altered consciousness, ataxia, and anterograde amnesia are present. Imaging features as areas of signal abnormality in the periaqueductal gray matter, tectal plate, and thalami are seen.
- Treatment
- No specific treatment. Secondary stroke prevention and memory rehabiliation are to be considered.