March 9, 2023
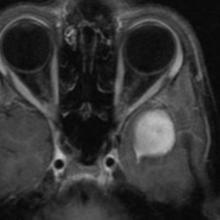
An 18-year-old man has a history of medulloblastoma detected in 2010. He received radiation therapy postexcision and developed recurrence in the form of dural metastasis along the left sphenoid wing in 2016, which was managed with chemotherapy and consolidation irradiation. In 2020, the patient presents with left-sided headache for 2 months and left temporal swelling for 1 month.